I
Parkinson’s disease is a chronic neuro-degenerative condition. In simple terms, this means that it lasts for many years, and involves the withering away of certain nerve fibers in the brain.
Recently, a dear patient of our clinic requested that I write an article on this clinical condition. Her husband had suffered from it for years before he passed. She just wanted a better understanding of this condition in order to come to terms with her loss.
I decided it would be appropriate for me to write a detailed guide. You are welcome to print this off and share it with people you think this might help.
Alternatively, just click any of the buttons above and below this article and share it with your friends.
Okay, now let’s take a look at this condition.
What Is Parkinson’s Disease?
Parkinson’s disease, or PD, was first described by
In simple terms, Parkinson’s disease is a condition where certain cells in the brain cease to function normally. This results in a number of symptoms which I have described later in the article.
In 2004, a door to door survey was conducted in Bangalore to find out how many people had Parkinson’s. It was found that around 33 people per 1 lakh population suffer from this problem.
Globally, it is estimated that there are around 10 million people who suffer from this problem.
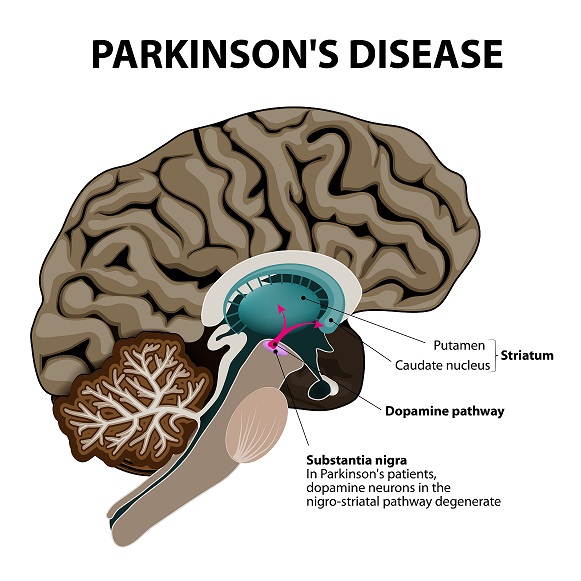
The primary problem in Parkinson’s disease is with a chemical compound in the brain called Dopamine in a part of the brain called the substantia nigra.
When produced in normal quantities, it helps control certain movements and actions that we perform on a day to day basis.
In PD however, the nerve cells (neurons) that produce dopamine fail to do so. This results in the clinical symptoms of the condition.
In addition to dopamine, there are other chemicals that may not be produced adequately. Once such example is norepinephrine. The extra symptoms that are seen is due to the low levels of this chemical.
Why Does One Get Parkinson’s Disease?
So, what causes Parkinson’s Disease?
In nearly 80% of cases, there is no cause identified. This is called
However, there are many other reasons why it might happen.
People who have poor blood supply to the brain, or those who have had a stroke in the past may develop PD.
Certain medicines prescribed for psychosis ( haloperidol, thiothixene, and risperidone) and for epilepsy may develop this condition as a side effect of
Exposure to environmental toxins may cause PD as well. However, this is quite rare.
The average age at which PD symptoms begin to appear is around 60 years. Less than 5% of patients present below the age of 40 years.
If a first degree relative suffers from it, then you are at a 2-3 times greater chance of developing PD.

If one were to look at the physiology behind this condition, research would show that the dopamine – p
Dopamine is a chemical that acts
For the symptoms of PD to appear, at least 80% of the nerves that produce this chemical must be damaged. This means that patients may only start to show symptoms when a large part of the brain is already affected.
In addition to just low levels of dopamine, there is also an alteration in a brain protein called alpha-synuclein. This alteration makes this protein a toxic one.
This ends up forming small Lewy bodies in the cells of the substantia nigra. The presence of these Lewy bodies in the brain is quite typical of this condition.
Other chemicals such as norepinephrine may also be present in low quantities.
Risk Factors for Parkinson’s Disease
The table below lists the common risk factors for PD.
2. Gender – Men are more likely to develop PD compared to women.
3. Environmental factors – Pollutants in the air (cyanide, carbon disulfide), the use of pesticides and chemicals; all increase the risk of developing PD.
4. Genetics – If you have a family history of PD, then you are a 2-3 times greater risk of developing the condition.
5. High body mass index
6. Head injury (example is Mohammad Ali, the legendary boxer)
7. High cholesterol levels
Despite these risk factors, it is never really clear what causes this problem. There is still a lot of research ongoing in this area.
I have mentioned above that advancing age is a risk factor for PD. While most patients above 60 years are at a risk, there are other forms of Parkinson’s that present at an earlier age.
Juvenile Parkinson’s Disease (rare) presents in individuals under the age of 21 years. Early onset PD is seen in people between 21 – 50 years.
Interestingly, smoking may lower the risk of the condition (that does not mean in any way that you take up smoking!). Caffeine intake is also linked to lowering of risk. These associations are not strong.
Symptoms of Parkinson’s Disease
PD presents with a triad of symptoms – tremors, rigidity and bradykinesia. I will explain these a little later.
However, the early symptoms of PD are quite non-specific.

For example, some patients may notice a change in their sense of smell. Constipation may be an early symptom as well. Disturbed sleep is a problem sometimes.
These symptoms may precede the actual symptoms of PD by years.
Let’s have a look at the actual symptoms of Parkinson’s Disease.
Tremors
This refers to a fine shaking of the arm, hand or jaw. It may also involve the tongue, lips, chin, and legs. It is present in 70 – 90% of patients.
Typically, the tremor occurs when the patient is at rest and relaxed. It has been described as a ‘pill rolling’ tremor. The tremor disappears when moving the affected limb and during sleep. It may worsen when under stress.
A tremor can be the first visible sign of PD. It generally affects one half of the body. However, as the disease progresses, it may affect both sides.
When assessing the tremor, doctors will sometimes ask the patient to close their eyes and count down from 100 to 1. When doing this, their mind is distracted and the tremor may become a lot more evident.
Rigidity
This refers to stiffness of the muscles of the arms or legs, and is seen in 80 – 90% of patients. When attempting to bend the arm, the movement is in the pattern of a cog-wheel.
In other words, there is stiffness that does not allow smooth movement of the muscles when they are being flexed.
This is called cog-wheel rigidity and is a classic sign of PD.
Bradykinesia
This refers to slowness of movement, and is seen in 80 – 90% of patients. The individual takes a lot longer to move and perform simple tasks.
For example, the patient will get up from the chair a lot slower than normal.
Other Symptoms
There are some other signs of Parkinson’s disease that patients can express.
One such problem is with posture and balance. Individuals may begin to stoop over and may have problems maintaining balance in an upright position due to this condition. Postural instability is seen in around 50% of patients within 5 years of diagnosis.
Another problem that they may notice is difficulty with certain automatic movements. This includes blinking and arm swinging when walking.
A change in the way the individual speaks may also be noticed. Example, there may be slurring of speech or even problems expressing words.
A change in the handwriting of an individual may be one of the early signs of this condition. In particular, the handwriting may become quite small. This is called micrographia.
When walking, patients may take short, small steps at a fast pace. This is called a ‘festinant’ gait. They tend to stop when there is an obstacle right in front of them. However, they rarely fall due to this alone.
Excessive sweating may be a symptom. Some patients may develop urine retention in the bladder.
With advancing disease, the facial expression of the affected person may change. In essence, it becomes expressionless or ‘masked’. This is called hypomimia.
Early, Hidden Signs Of Parkinson’s Disease
There are certain signs that appear very early on that can be considered to be hidden clues for Parkinson’s disease.
For example, some individuals may notice pain in the shoulder or dragging of a leg that does not improve when steroid injections are given. Difficulty turning in bed may be noticed.
Some patients may develop a softness in their voice, making it inaudible over the phone.
The signs are subtle and can only be diagnosed by a neurologist. Please don’t jump to conclusions should you encounter anything like this.
Stages of Parkinson’s disease
As Parkinson’s disease is a progressive condition, it develops in stages. Clinically, there are five stages that are present in the progression of Parkinson’s disease.
Stage I
In stage I, the bottom of the brain i.e. the medulla is attacked by the clinical condition. Individuals begin to experience constipation and may even lose their sense of smell. The symptoms can take place decades before the actual classic textbook symptoms of Parkinson’s disease develop.
Stage II
In this stage, there is deterioration of the health of the nerves in the message centre of the brain i.e. the pons.
This leads to symptoms of depression and may even cause trouble sleeping. Rarely, people may even act out their dreams when they are asleep and hurt themselves in the process.
Stage III
In this stage, the symptoms of tremors and a short shuffling walking pattern appear. This is because the part of the brain that is responsible for movement is now affected.
Stage IV and Stage V
This is the advanced level of Parkinson’s disease. Not only is their movement disorder a problem but also associated with this is memory loss (dementia) and hallucinations.
Complications of Parkinson’s Disease
As I have already discussed in the article earlier, one complication of Parkinson’s disease is memory loss.
Some individuals may have problems remembering certain simple things and may also experience difficulties making decisions.
Unfortunately, this change does not respond to medical therapy.
Clinical depression is a common complication and can worsen prognosis in individuals with PD. Consultation with a psychiatrist and commencement of antidepressant medication may help the patient to some extent.
Dysphagia, or swallowing difficulties, may become a problem. Not only that, there may be problems with the way the chewing muscles of mouth work, making it difficult to eat food.
Over a period of time, the lack of sufficient amount of food intake can lead to weight loss and overall weakness. Since swallowing becomes hard, any saliva that is produced in the oral cavity may begin to drool out of the mouth.
Incontinence of urine and trouble controlling bladder function is a complication of this condition. Bowel issues such as constipation may also occur.
Blood pressure changes may be noticed in advanced disease. Patients may experience a drop in blood pressure when standing up from a sitting or lying position. This may lead to falls as well.
Sexual dysfunction may become a problem, with some patients losing their sexual drive.
Finally, sleep disturbances are extremely common in advanced Parkinson’s disease. Patients may wake up in the middle of the night and begin walking around in a hallucinated state. Medication is required to help patients sleep in such a situation.
Diagnosing Parkinson’s Disease
There are no specific tests that can help confirm a diagnosis of Parkinson’s disease.
Neurologists diagnose this condition by evaluating the symptoms and eliciting the signs.
MRI scans, PET scans and similar studies bear little value in management of the condition. However, they may be performed to rule out any other condition that is suspected.
Treatment Of Parkinson’s Disease
Medical therapy in the form of tablets is the mainstay of treatment. There are also certain surgical treatments that may help relieve symptoms. Unfortunately, the condition is progressive, and all the tablets do is control the symptoms and prolong life to some extent.
There is no cure for Parkinson’s Disease.
Medical Therapy
The medicines that are prescribed in the treatment of PD are primarily aimed at increasing the levels of dopamine in the brain. This

The primary drug that is used in the treatment of Parkinson’s disease is levodopa, also called L-Dopa.
As I have explained previously, this condition is typically
Sometimes, patients taking levodopa may also be given another drug called carbidopa. This additional medication can help reduce the side effects of levodopa therapy. In India, this combination is available as Syndopa.
The dose of levodopa is started at low levels to begin with and this is increased gradually as per the patient’s response. The medication should never be stopped without seeking a doctor’s approval. If the medicines are stopped suddenly, patients may experience serious side effects such as entire body stiffness and sometimes even breathlessness.
Other medications that may be prescribed are mono-amino oxidase B (MAO-B) inhibitors. These are drugs that block the activity of an enzyme that is responsible for the breakdown of dopamine in the brain. Similarly, another group of drugs called catecholamine 0-methyl transferase (COMT) inhibitors may also be prescribed.
Generally, patients stabilise on one medication. However, as the disease progresses, they may require additional treatments.
Are there any side effects?
In around 4% of patients, dopamine dysregulation syndrome may develop. This is a condition where patients become addicted to treatments, leading to an increased use of medication when it has not been prescribed.
Around 15% of patients develop a condition called ‘punding‘ – a phenomenon where the individual begins to perform repetitive, purposeless actions such as sorting out or disassembling objects.
Deep Brain Stimulation
This is a relatively new therapy where tiny electrodes are implanted in the brain and attached to a small electrical device that is implanted in the chest.
This electrical device generates small electrical currents then go on to stimulate these parts of the brain where the electrodes are implanted. This may stop some of the movement problems associated with Parkinson’s disease.
Generally, this therapy is reserved for patients who have good cognitive function, who respond well to levodopa and those under the age of 70 years. Having a tremor resistant to treatment may require deep brain stimulation as well.
Deep brain stimulation therapy has its uses, and has been found to be as effective as levodopa therapy at its best. Patients may notice a sustained benefit for around 10 years or so. However, it is a costly procedure and has a few risks such as infections etc.
Physiotherapy and Occupational Therapy
Physiotherapy and Occupational Therapy at an extremely important part in the management of PD.

By helping patients maintain independence, the disease becomes a lot more easier to handle. Physiotherapy has to be continued, and evidence suggests that stopping physiotherapy may halt any progress.
Exercise is obviously good in keeping the patient active, but there is no evidence it improves the functioning of the brain.
Speech therapy has a role as well, helping improve voice quality.
There are a number of newer treatments being investigated for Parkinson’s Disease. However, they are very complex and are out of the scope of this article. If you wish to read more, click here.
Information For Carers
Carers of patients with PD are usually family members, who rarely have the training needed to take care of the affected individual.
At times, managing them can be quite frustrating. There are 2 reasons for this –
- The constant need for attention and help can totally disrupt the life of the carer. They rarely get time for themselves.
- Seeing someone they love suffer gradually and over years can be heart-breaking as they feel helpless.
In the early stages, patients rarely require support and help. Medications do a good job controlling symptoms, and they are able to perform almost all activities with reasonable independence.
However, patients who receive a diagnosis of PD may express a variety of emotions. This can range from anger to frustration and low mood. ‘Why me?’ is something that they constantly ask, having lived a life by the rules.
As their carer, help them maintain a positive attitude. Emotional support of such patient goes a long way in helping them cope with the changes they are experiencing.
Make sure you have a good knowledge of the medication the patient is taking. They may forget it, so remembering exactly what they are taking and when they are taking it can help ensure they take their medicines on time and regularly.
Just because your loved one has now been diagnosed with PD does not mean the tow of you cannot do together what you enjoy. Make sure you spend time together – have outings, spend a romantic evening together – anything is possible.
Try and maintain social connections and friendships. This will help offload some of the stress you might be feeling caring for the patient. It is important that your state of mind is good if you have to take care of a loved one with Parkinson’s Disease.
Closing Remarks
Parkinson’s Disease is a progressive condition that can unfortunately rob the affected patient of their dignity over years. However, there are treatments available that can help keep symptoms under control and help maintain quality of life to some extent.
- Understanding Iron Deficiency Anemia: A Guide for Patients - May 31, 2025
- CT Coronary Calcium Score: A Guide for Patients - January 7, 2024
- Gastric Antral Vascular Ectasia (GAVE) – Causes, Diagnosis, and Treatment - August 5, 2023


Thank you Vivek for writing about PD . I’ve been on medication for it , now for 3 yrs . 4 yrs since I knew something was wrong with me . Started with a tumour in my spine .. surgery for it and eventually being diagnosed with PD .
Have also read numerous articles on the net about PD . Right now need no help and can manage well myself but I know it’s progressive. I hope for the best and pray I don’t become a bad case .
Kanaka ( hope u remember me )