COVID-19 infection rates are soaring rapidly in our country. In the last week alone, I have had over a 200+ calls and many more text messages about patients or their relatives/friends who have contracted the virus.
It is disheartening and deflating to say the least to see so many people suffering from an infection caused by an organism we can’t even see.
Those who have been calling the medical community and visiting hospitals are being evaluated to see whether they can be quarantined at home or if they need hospitalisation.
I thought I would explain to you how patients are being treated in both settings.
Grab a cup of coffee as this is going to take a while.
The COVID Report
There are 2 types of COVID tests being done at the moment.
COVID RT-PCR Test – This is the ‘Reverse Transcriptase – Polymerase Chain Reaction’ test. It is the most commonly performed test that takes around 48 hours for results. With the rising cases, the time taken has gone up to nearly 5 days.
Antigen Test – This looks for the viral antigen protein fragments, and the reports are given within a few hours (sometimes within 30 minutes). However, if positive, it is still confirmed with an RT-PCR test.
Let’s look at the RT PCR Test as this is done most frequently.
COVID -19 RT PCR Test
The RT PCR test is a test where the genetic sequence of the Sars COV virus is mapped out and sequenced. The material is amplified many-fold so that the genetic material can be detected through the test.
Four genes are detected through this test –
- RdRP gene – This is the RNA dependent RNA polymerase gene
- Structural protein gene E (detects the envelope of the virus)
- Structural protein gene N (detects the nucleocapsid of the virus)
- ORF1 ab gene – Also called the open reading frame 1a and 1b
I know, it’s a little too complicated, so I will refrain from any further discussion on this. The only reason I have mentioned it is because you will see this in some of your reports.
Despite such a detailed test, the result is rarely 100% accurate. In fact, it can miss 3 out of 10 cases (70% sensitivity), but when positive it is 95% accurate (specificity).
This disparity in results is not due to the test itself, but also depends on how the sample is collected, cross-contamination and local expertise on accurate collection methods. The duration of symptoms and the severity of the illness are also factors.
When the virus mutates, which it has, the reports can be falsely negative.
If the sample is collected too early on in the disease, the result can be falsely negative. This means that while you are exhibiting COVID symptoms, your test will be negative.
In such circumstances, if clinical suspicion is high, I have advised repeat testing in 3 to 4 days.
Interpreting RT PCR Report
When you look at an RT-PCR report, you will see values like CT value. CT value stands for Cycle Threshold value. The value is inversely proportional to the viral burden in the body.
In RT PCR testing, a small amount of the virus is put through multiplication cycles in order for it to be detected. If fewer cycles are required to detect the virus, it means the viral load is very high.
This is what a COVID report might look like.
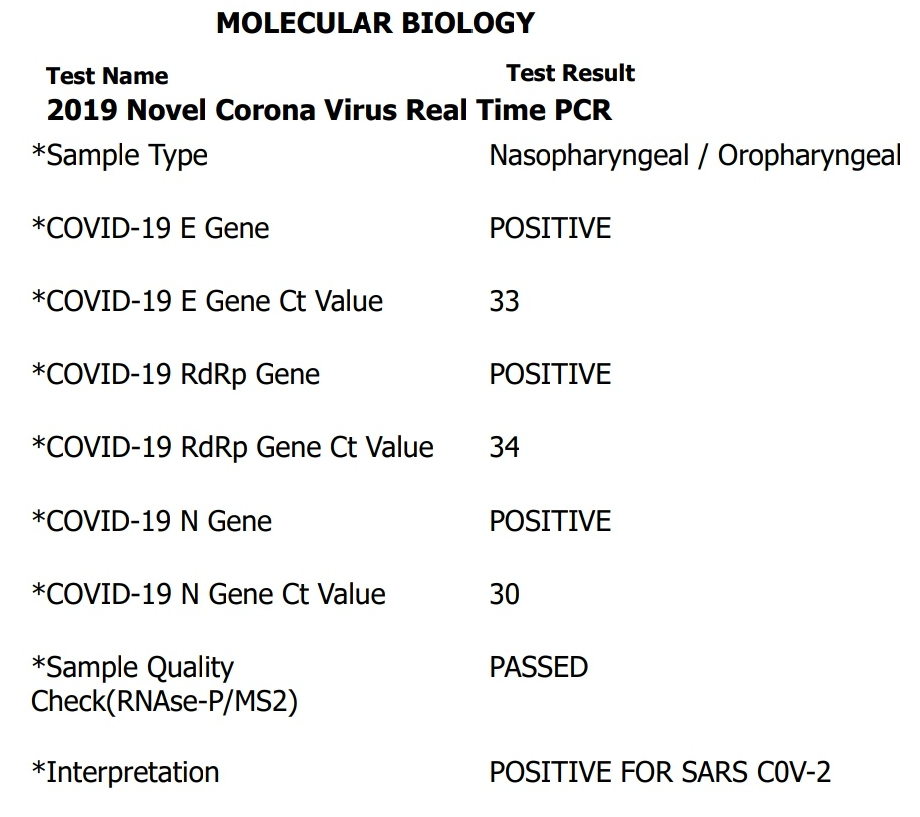
If the CT value is below 25, the quantity of the virus in the body is high. If the value is equal to or above 35, it indicates a mild infection or no infection. Values between 26-34 indicate moderate infection. Unfortunately, these values are not standardized, so don’t delve too much into it.
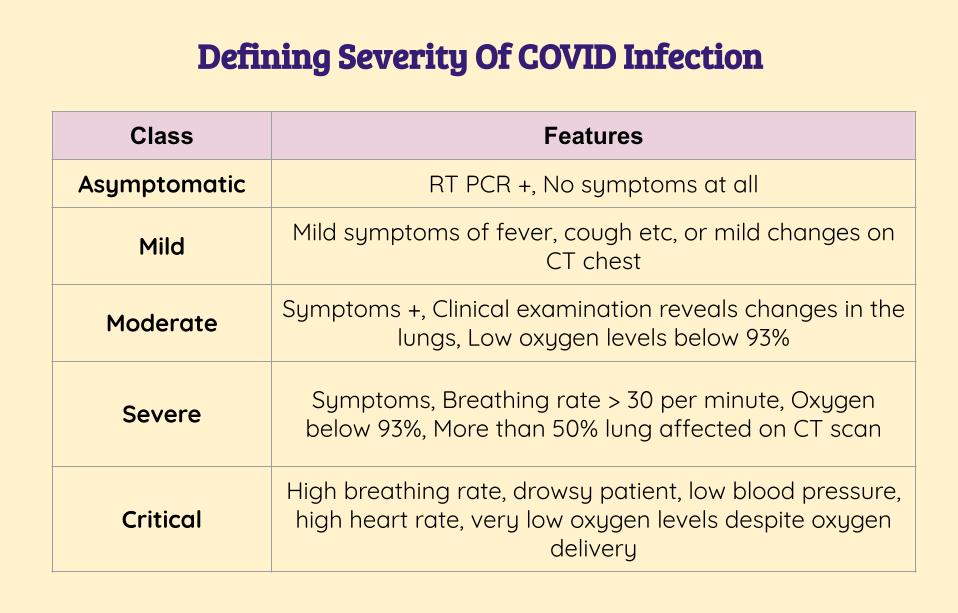
Severity Of Illness
Blood Tests
If you are positive for Sars CoV infection, you may be asked to undergo certain blood tests. These include a complete blood count, C-Reactive Protein (CRP), ferritin, D-Dimer, Lactate Dehydrogenase (LDH) and Interleukin-6 (IL-6).
You may not need to undergo all these tests though.
I will discuss a few here.
C – Reactive Protein (CRP)
CRP is basically a protein that is produced by the liver in response to inflammation. It is not a specific test to COVID infection, and values can also go up in arthritis and infections.
In COVID infections, the CRP value is one of the first ones to increase.
A high CRP value is indicative of the severity of the illness. In one clinical trial, a value above 41.8 mg/L was a determinant in progression of mild illness to severe disease.
Interleukin-6 (IL-6)
You may have read of the ‘cytokine storm’ that accompanies COVID infection. This is basically a rush of inflammatory products that are released into the bloodstream after contracting the infection.
IL-6 is the most common cytokine that is released into the blood. In severe cases, the levels can be almost 3 times higher than they are in mild cases.
While it’s effect is still being studied, having very high IL-6 levels could indicate more severe disease.
IL-6 levels are not routinely measured as the test can be quite expensive. There are cheaper markers that can help determine severity.
D-Dimer
In simple terms, D-dimer test helps determine how thick the blood has become as a result of the infection.
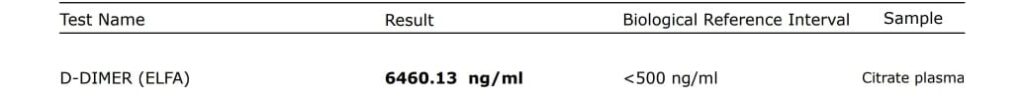
High levels of D-dimer are considered a marker of bad outcomes. High levels also indicate severe disease.
Very high D dimer levels sometimes indicate the risk of developing blood clots in the lungs. This is called pulmonary embolism. Pulmonary embolism is a potentially life threatening problem.
If your D-dimer levels are elevated, chances are your doctor will advise you blood thinners to prevent these blood clots from forming. Usually Aspirin is what is given. If levels are higher, you might be started on stronger agents like Dabigatran or Rivaroxaban.
Ferritin
This is a marker of inflammation. The higher the levels, the more severe the condition.
Complete Blood Count
A complete blood count checks your hemoglobin, white cell count and platelet count.
The white blood cells include cells called neutrophils (your soldiers against bacterial infections), lymphocytes (also fight viruses and bacteria), eosinophils (fight allergies(, basophils and monocytes.
In COVID infection, neutrophils rise, while the other values fall. The ratio of neutrophils to lymphocytes indicates the severity of the illness.
The higher the value, the more severe the illness. A ratio of neutrophil/lymphocyte >3.13 is considered to be severe and have a worse prognosis.
Platelets are cells that are responsible for clotting of blood. A low platelet count in COVID infection is also an indicator of poorer outcomes.
Cardiac Troponin
In severe cases, a cardiac troponin test will be done. This is a protein that is released into the bloodstream when there is damage to the heart muscle from the virus.
It is the same protein that is elevated in value in a heart attack.
The test, while has some uses, is not often performed as it could lead to inappropriate cardiac consults and investigations.
2. Thermometer – You can use an infrared thermometer or a digital one (for single person use only)
3. Blood pressure monitor
4. Glucometer if you have diabetes
CT Imaging
CT scan imaging of the lungs is being performed for almost all patients with COVID infection, or with suspected infection.
In early stages, the CT findings in the lungs, called ‘ground glassing’, may be minimal. As the disease progresses, the score will increase. Starting treatment at the right time is key to prevent this progression.
The image below shows a patient who have florid COVID infection in the lungs.
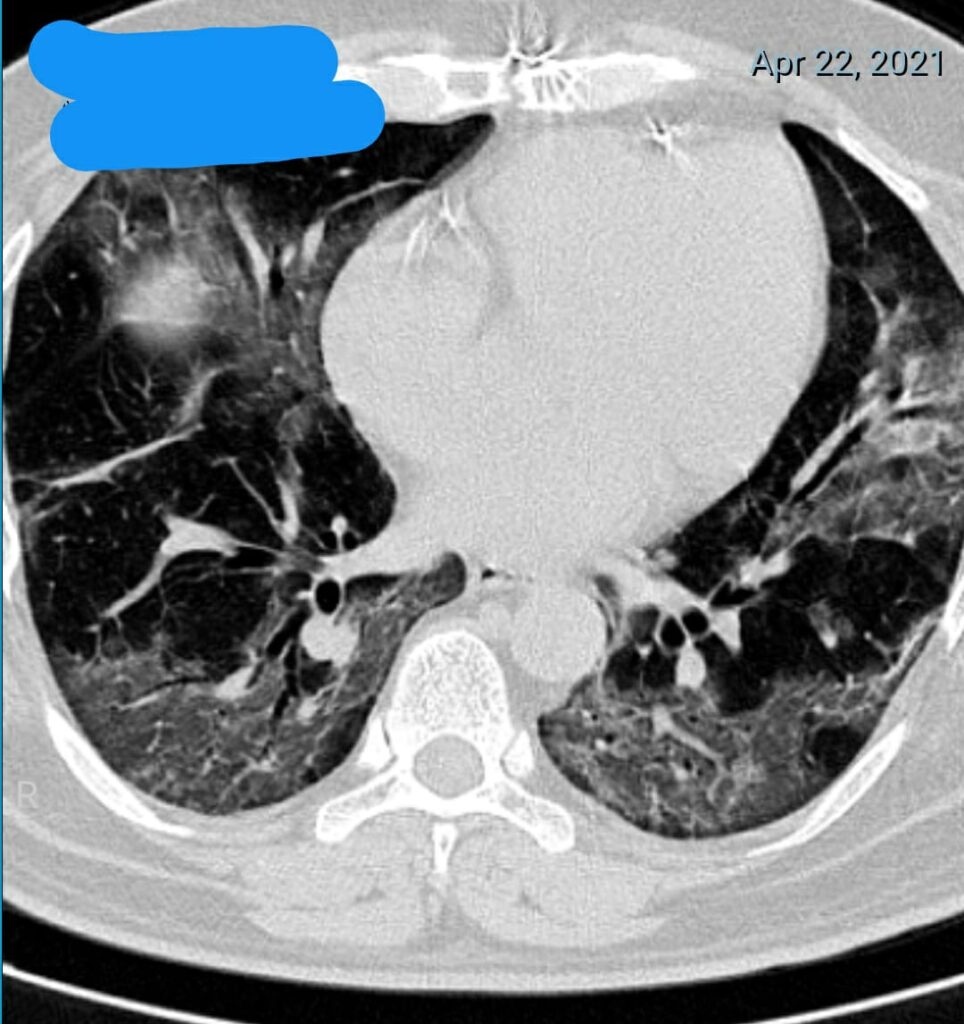
CT scoring is conducted during all CT chest scans. A score of less than 8 indicates mild involvement, 9-15 indicates moderate involvement, and 16 – 25 indicates severe involvement. The patient above has a score of 16.
Do note that having mild lung involvement does not necessarily mean all is okay. The disease can progress, and treatment will be given based on the presentation of the patient.
Symptoms and Prevention
This image below says it all. Fatigue, loose stools, abdominal pain and headache can also be symptoms.

Treatment For COVID Positive Patients With No Symptoms
If you have gotten a test done and you have absolutely none of the symptoms listed in the table above, then it is unlikely you will be given any treatment at all.
You will be asked to quarantine for 14 days or as per the local guidelines.
If at any point you develop symptoms or your oxygen levels begin to drop below 94%, you will need to seek medical attention.
In asymptomatic cases, you can call your local hospital helpline to see if they have home care packages. For example, in Bangalore, Aster RV hospital and Fortis Hospital have a home care package. Details are in the images below.


- Increasing breathlessness
- Worsening cough
- Increasing heart rate over 100 beats per minute. You may experience palpitations.
- Lowering of oxygen saturations below 94%
- Lowering of oxygen levels > 4% when walking continuously for 3 to 6 minutes
- Neutrophil:Lymphocyte ratio of > 3.5
- Worsening of other symptoms
Treatment For COVID Positive Patients With Mild Disease
If you have mild disease, then you will be started on treatment. Protocols keep changing, and antibiotics, antihistamines and antiviral drugs will be prescribed.
You will be asked to check the severity markers – D-dimer, ferritin, CRP etc. Depending on this, further medicines will be prescribed.
The prescription will be long and daunting, and taking all the meds will likely cause gastritis. But stick with the treatment as much as you can to avail whatever benefit it will give you.
The common drugs that are being prescribed are Doxycycline, Ivermectin, Azithromycin, cetirizine and cough syrups. Paracetamol is being prescribed for fever. Multivitamins (C, D) and Zinc will also be prescribed.
I am not including the doses for each here. Please contact your doctor for the relevant prescription.
Please note that none of these drugs have been clinically proven to completely cure COVID. All of them have some effect in lowering the intensity of the infection. The body is the one that is going to fight the infection.
If your oxygen levels begin to drop, then laying on your chest and doing some deep breathing can help. This is called ‘prone breathing’ and allows the lungs to expand to a greater extent. This allows more oxygen into the lungs.
Essentially, if you are in good health and have taken care of your well being over the years, then it is highly likely you will get through it easily.
Those who are overweight, have diabetes, cardiac disease or any other such chronic medical conditions are at a higher risk of developing severe infection and must observe every precaution possible to prevent picking up the infection.
If you are negligent and feel that you are invincible, think again.
If you do catch the virus, you may be at risk of severe infection which could be life threatening. I’m not joking here.
Treatment For COVID Positive Patients With Severe Disease
In addition to the regular treatments that are being administered to patients, those with severe illness require ICU care or ward based management, depending on their markers and oxygen needs.
- D – Dimer > 1000 ng/mL
- CRP > 100 mg/L
- LDH > 245 units/L
- Troponin > 2 times the upper limit of normal
- Ferritin > 500 mcg/L
Patients will undergo a CT scan of the chest, an arterial blood gas analysis, blood investigations and severity marker tests. These tests will be repeated either daily or every 48 hours.
Oxygen levels will be monitored regularly. Treatment will be administered to ensure oxygen levels are above 95%. Simple oxygen alone can be delivered to the patient on a ward.
If normal oxygen delivery mechanisms such as a mask or nasal cannula are ineffective, then you may be advised high flow nasal cannula (HFNC) non-invasive ventilation.
This decision is made based on the ROX index, which looks at the ratio of the oxygen saturations to the breathing rate of the patient. If the value is less than 4.8, then shift to ICU is advised for non-invasive ventilation.
Non invasive ventilation, or NIV, is a pressure operated mask that pushes oxygen into the lungs while allowing the patient to breathe out carbon dioxide. It is attached tightly to the face, and is not very comfortable.
However, once attached, you will get used to it in a few minutes. Patients will on occasion be ventilated in the prone position to allow better oxygen entry.
Along with oxygen therapy, patients will be started on antibiotics, intravenous Remdesevir and intravenous steroids. Blood thinners in the form of Heparin injections or tablets will be given.
Antibiotics
The antibiotics given are broad spectrum antibiotics that cover all bacterial infections. These are given as during severe COVID infection, the patient becomes vulnerable to secondary bacterial infections.
Remdesevir
Injection Remdesivir has gained popularity, and I am sure you have already heard of it. It is given to attempt to hasten recovery, but clinical data suggests that using it does not lower the chance of patients succumbing to the disease.

Remdesivir is avoided in patients with advanced kidney disease. Liver side effects exist, and liver function will be monitored when in hospital.
Steroids
Dexamethasone, an injectable steroid, is invaluable in the treatment of COVID infection. Oral steroids such as methylprednisolone, prednisolone and hydrocortisone are also used if the oxygen levels are low or the patient is heading towards ventilation. They can be life-saving.
Patients started on steroids will notice a fluctuation in their blood glucose levels, particularly if they have diabetes. There is also a risk of infections as well, so antibiotics will be prescribed.
Steroids have been shown to lower mortality in patients with severe COVID.
Heparin Injections
Heparin is a blood thinner, and prevents the formation of blood clots in COVID. In the last years, a few cases that have succumbed to COVID infection have been due to large blood clots within the lung. This is called pulmonary embolism and is life threatening if it occurs.
Tocilizumab
This drug is a drug that lowers the levels of Interleukin-6 by blocking the receptors it attaches to. It is recommended for those patients who have very high D-dimer levels, ferritin levels and IL-6 levels.
It is also recommended for those who have oxygen levels < 92% and CRP values above 75 mg/L, along with those on some form of respiratory support.
The drug is used in conjunction with steroid dexamethasone in the ICU. However, if the patient has very low immunity, then the drug will be avoided.
It is currently unavailable – out of stock – in India.
Convalescent Plasma Therapy
This is also reserved for patients with severe disease in the ICU. It is basically plasma that has been derived from patients who have recovered from the illness. This plasma is rich in antibodies that are believed to fight the COVID virus.
Unfortunately, it does not have much benefit in lowering mortality, and may not be of much benefit in severe disease.
Extreme Cases
In the event that the patient deteriorates, a decision will be taken to ventilate the patient using a ventilator.
This is offered to patients whose oxygen levels do not improve despite all the above treatments.
Prognosis
Most cases of COVID-19 get better. But this year we have seen patients taking a lot longer to recover.
Patients who require ICU and ventilation (with a tube in the lungs) carry a bad prognosis. Our experience in this area is extensive, and many times teams will do their best to avoid attaching the patient to a ventilator.
Final Note
COVID IS NOT A JOKE. PLEASE TAKE IT SERIOUSLY.
I still see people roaming around in groups on their walks, chit chatting away like all is well in the world. It’s time to wake up and realize that it is not.
There is no use sitting and panicking about it, and then being reckless about it by not observing the precautions that are essential to prevent spread.
Even now, I see people meeting up at their local coffee shop for a chat and coffee. It is beyond me as to why they can’t just avoid that. You can have your coffee at home.
Remember, this virus differentiates against no one. You are not invincible. You are just as likely to get it as the person who is waiting outside a hospital gasping for breath as there are no beds.
Please take COVID infection seriously. It is easy to prevent yourself from contracting it. Masks, hand washing, social distancing, avoiding large gatherings and venturing out of the house if absolutely necessary should be observed.
Please take care of yourself. I wish you all good physical and mental health. I hope you found this article helpful. If you have any questions, please do write them in the comments section below and I shall answer them.
- CT Coronary Calcium Score: A Guide for Patients - January 7, 2024
- Gastric Antral Vascular Ectasia (GAVE) – Causes, Diagnosis, and Treatment - August 5, 2023
- Understanding Xanthelasma: Causes, Symptoms, and Treatment Options - June 28, 2023


Thank you for a detailed analysis.No Doctor has done this well so far.
You are really great and your service to society is commendable.
I have one question :
Is the current Virus Airborne?
Why India is not able to prevent death due to man made calamities like in Delhi oxygen shortage?
Thank you Dr. Vivek Baliga🙏🙏🙏
I have gone through your message… Any person with a little bit of medical knowledge can understand your article on Covid….
Really it’s very very useful article to know about Covid and the sufferings of Covid patients….
General public should understand the ground reality
and should Stay at Home and should leave the home except in emergencies..
STAY HOME STAY SAFE
PREVENTION IS BETTER THAN CURE
THANK YOU ONCE AGAIN DOCTOR…
Very Very informative
Thanks a lot
Thank you for the detailed information, doctor.
An excellent document doctor. Thank you so much. Hats off to you in finding time and writing such well researched article. Your concern and involvement in our care is touching…. Thanks again….
Thank you, Dr.Vivek Baliga, I am your patient, this is the most comprehensive article I have come across on Covid19. Request you to add information regarding vaccines and address people’s apprehensions regarding the same.
Excellent job Sir. Really detailed, helpful and relevant article.
Dr, your article is very informative . Is there a possibility that you can use your good offices and organise a vaccination camp for your patients and families. It would be of great help. Any thoughts?
Thanks
Balakrishna Shenoy